Obsessive Compulsive Disorder affects individuals across all walks of life, yet many wonder exactly how it manifests, evolves, and responds to treatment.
Therefore, this article will guide you step by step through the essential aspects of Obsessive Compulsive, from its definition and prevalence to its types and severity levels. By explaining how each feature influences daily living, you will gain a practical understanding that goes beyond mere definitions.
Table of contents
- Introduction
- 1. How Common Is Obsessive Compulsive Disorder?
- 2. What Types of Obsessive Compulsive Exist?
- 3. What Misconceptions Surround Obsessive Compulsive?
- 4. How Do Researchers Study Obsessive Compulsive Disorder?
- 5. How Can Communities Support Individuals with Obsessive Compulsive Disorder?
- 6. Conclusion: How Can We Rethink Obsessive Compulsive Disorder?
- references
Introduction
Obsessive Compulsive Disorder often begins in late childhood or early adulthood, although children as young as seven can exhibit symptoms. Although researchers estimate that roughly 2% of people worldwide will experience obsessive compulsive at some point, the intensity and impact of symptoms differ markedly from person to person. In this introduction, we answer the question how OCD shapes thoughts and behaviors. We also outline the questions that guide this article—so by the end, you will know exactly how to recognize, assess, and support someone living with obsessive compulsive.
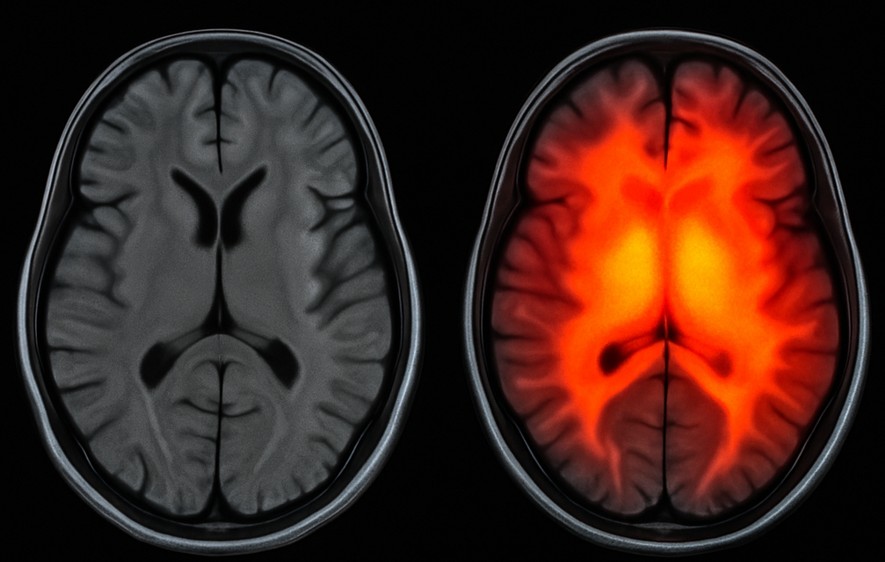
Healthy vs. Hyperactive OCD Brain MRI
The red overlay marks regions of excessive neural activity—particularly in the frontal-striatal circuits—indicating the hyperactive brain areas commonly seen in OCD.
1. How Common Is Obsessive Compulsive Disorder?
1.1. How Do Prevalence Rates Vary by Region and Time?
Although obsessive compulsive occurs worldwide, rates differ depending on survey methods and cultural context. For example:
- In the United States, studies show a lifetime prevalence of approximately 2.3%, with a 12-month rate around 1.2% nimh.nih.gov.
- A recent meta-analysis pooling data from 34 countries found a global lifetime rate of about 1.3% and a 12-month rate near 1.1% ScienceDirect.
- Meanwhile, some Asian surveys report lifetime rates up to 3%, although differences in diagnosis criteria may play a role Crown Counseling.
These figures reveal that, although measurement methods vary, obsessive compulsive consistently ranks among the top four mental health conditions worldwide.
1.2. How Does Age of Onset Influence Prevalence?
Obsessive compulsive can appear at almost any age, but research highlights key patterns:
- Childhood-onset (before age 10) accounts for about 20% of cases, especially in boys (AAFP).
- Adolescent-onset (ages 11–19) is the most common, with symptoms often persisting into adulthood.
- Adult-onset after age 35 is rare but does occur, frequently linked to significant life stressors such as loss or major illness.
By understanding these age-based trends, caregivers and clinicians can tailor screening and early-intervention strategies more effectively.
2. What Types of Obsessive Compulsive Exist?
2.1. Which Symptom Subtypes Appear Most Often?
Researchers classify obsessive compulsive symptoms into several subtypes, each reflecting a core theme of obsessions and compulsions:
- Contamination & Cleaning
How it shows up: Repeated handwashing, avoidance of “dirty” objects, excessive showering.
Why it matters: These rituals can consume hours per day, leading to skin damage and social withdrawal. - Symmetry & Ordering
How it shows up: Aligning items perfectly, counting actions, discomfort if arrangements feel “off.”
Why it matters: Disruptions in routine or environment spark intense distress, making travel or shared spaces challenging. - Checking
How it shows up: Verifying locks, appliances, or one’s own memories.
Why it matters: These rituals can delay leaving the house, arriving late at work, or missing social events. - Forbidden Thoughts
How it shows up: Intrusive violent, religious, or sexual images; mental rituals to “undo” these thoughts.
Why it matters: Sufferers often feel ashamed and avoid seeking help, believing their thoughts define them. - Hoarding
How it shows up: Difficulty discarding items of no value, fear of future need, clutter that disrupts living spaces.
Why it matters: Hoarding can pose health risks, strain relationships, and reduce living quality.
By recognizing these subtypes, you can ask targeted questions that reveal which manifestations trouble someone most deeply.
2.2. How Is Severity Measured in Obsessive Compulsive?
Clinicians commonly use the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) to quantify severity. The table below shows how scores translate to severity levels:
| Y-BOCS Total Score | Severity Level |
|---|---|
| 0 – 7 | Subclinical / Mild |
| 8 – 15 | Mild |
| 16 – 23 | Moderate |
| 24 – 31 | Severe |
| 32 – 40 | Extreme |
- Step 1: Clinician rates obsessions and compulsions separately on a 0–4 scale.
- Step 2: Summing yields the total Y-BOCS score.
- Step 3: Scores guide treatment planning; for example, moderate cases often begin with therapy alone, whereas severe cases may require combined therapy and medication.
By using this scale, practitioners ensure that treatment intensity matches symptom burden, which improves outcomes.
3. What Misconceptions Surround Obsessive Compulsive?
3.1. Is OCD Just About Being “Neat and Organized”?
No. Although symmetry and ordering represent one subtype, obsessive compulsive goes far beyond preferring tidy rooms. People living with OCD:
- Experience distressing intrusive thoughts that they cannot control.
- Perform rituals to alleviate anxiety, rather than for aesthetic reasons.
- Often recognize their actions as unreasonable but feel powerless to stop.
Therefore, labeling OCD as mere perfectionism minimizes the genuine suffering involved.
3.2. Can “Strong Willpower” Cure OCD?
Unfortunately, no. Obsessive compulsive disorder arises from complex brain circuitry differences, genetic factors, and learned responses. As a result:
- Simply “trying harder” rarely reduces intrusive thoughts or rituals.
- In contrast, Exposure and Response Prevention (ERP) teaches individuals how to face fears without compulsions, gradually rewiring anxiety responses.
- Medications such as SSRIs can alter serotonin pathways, further enabling progress in therapy.
Thus, OCD demands a structured approach rather than willpower alone.
4. How Do Researchers Study Obsessive Compulsive Disorder?
4.1. What Methods Help Us Understand OCD?
Researchers use a blend of tools to decode the puzzle of obsessive compulsive disorder:
- Brain Imaging (fMRI, PET scans):
Shows overactivity in certain brain loops (especially the orbitofrontal cortex, caudate nucleus, and thalamus).
➔ Creatively speaking: Imagine a broken traffic light at a busy intersection — thoughts keep looping with no green light to move forward. - Genetic Studies:
Reveal that first-degree relatives of someone with OCD have a twice higher risk of developing it.
➔ Non-traditionally thinking: Genetics aren’t destiny — they are a canvas, not a blueprint. - Behavioral Experiments:
Show that avoidance and compulsions, while short-term soothing, long-term strengthen the fear circuit.
➔ Progressive view: OCD isn’t about “weirdness” — it’s the brain accidentally learning the wrong lesson too well.
Through these approaches, science reframes OCD: not a character flaw, but a rewritable brain story.
5. How Can Communities Support Individuals with Obsessive Compulsive Disorder?
5.1. How Should Friends and Families Respond?
If someone you know lives with obsessive compulsive disorder, your role can be quietly revolutionary. Here’s how:
- Listen without judgment: Avoid saying “That’s crazy” or “Just stop.”
- Avoid enabling rituals: Compassion doesn’t mean helping them “check” the door one more time.
- Encourage professional help: Normalize therapy and medication, don’t treat them like a secret.
🌱 Progressive idea: Think of yourself as a co-creator in their healing — offering a space where growth, not fear, blooms.
5.2. How Should Schools and Workplaces Adapt?
Educational and professional environments can either crush or champion people with OCD. Leading institutions:
- Offer flexible deadlines for those coping with intrusive thought spirals.
- Train staff to recognize mental health needs early.
- Foster culture where vulnerability is strength, not stigma.
✨ Unconventional suggestion: Introduce “Mental Health Days” for employees and students — no justification required, only self-care.
6. Conclusion: How Can We Rethink Obsessive Compulsive Disorder?
Obsessive compulsive disorder isn’t simply a clinical diagnosis tucked away in textbooks. It’s a deeply human experience of grappling with uncertainty, fear, and hope.
Here’s how we move forward:
- See OCD not as a limitation, but a challenge to creativity — finding new ways to live with uncertainty.
- Advocate for early intervention so fewer lives are derailed.
- Replace shame with solidarity — a world where asking for help feels natural, not taboo.
If we collectively step beyond stereotypes, invest in science, and prioritize compassion, obsessive compulsive disorder will no longer be a silent thief of life. Instead, those who carry its weight can also carry a banner of resilience — and even brilliance.
references
- Healthline – Obsessive Love Disorder: Symptoms, Causes, and Treatment, written by Kimberly Holland, medically reviewed by Timothy J. Legg, PhD, PsyD (2020).
- Medical News Today – What is obsessive love disorder?, authored by Zawn Villines (2020).
- Verywell Mind – Understanding Obsessive Love Disorder, by Arlin Cuncic, MA (2021).
- Psychology Today – Obsession: The Psychology Behind Obsessive Love, various contributors (updated regularly, latest 2023).


















